The usual definition of ‘infertility’ is ‘the inability to conceive within 12 months of trying’. This is perhaps a useful rule-of-thumb but is far too simplistic. There is little relevance, for example, of ‘12 months’ to a woman with totally occluded (blocked) fallopian tubes. The simplistic definition is also found wanting when we consider the implications as to whether the couple are trying for the first time or have previously proven their fertility.
A better way to approach the dilemma of a definition is to try to put all this in context by defining what is ‘normal’ fecundity (the ability to conceive) in humans and then try to quantify the effects of common factors and consider their impact on the ability of a couple to achieve a pregnancy. Worldwide there does appear to be increasing infertility but the statistics are somewhat confused, not the least by better reporting in the developing world where sexually transmitted diseases and puerperal (after birth) infections contribute enormously to the problem. In developed countries the increase is far less apparent and the data less convincing. What we can say without argument is that it is not decreasing.
In western society the incidence of reported ‘delays in conception’ is around 10-15 per cent. We can expect approximately 88 per cent of those wishing to fall pregnant will conceive within 12 months and 30 per cent of the remainder (i.e. another 4 per cent) in a further year. Beyond this the expectation drops in the next year to around 10 per cent of the remainder, and 5 per cent the year after.
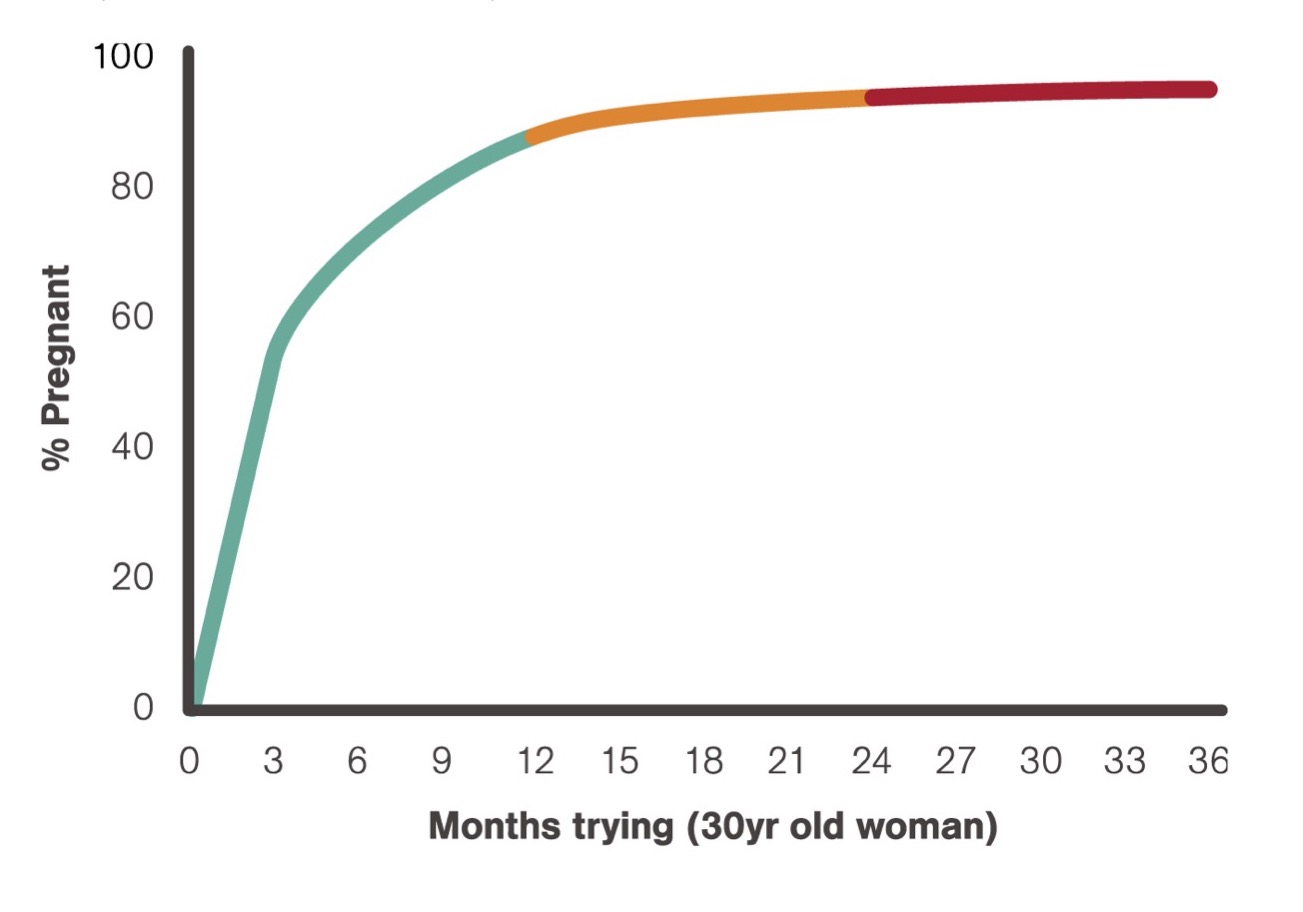
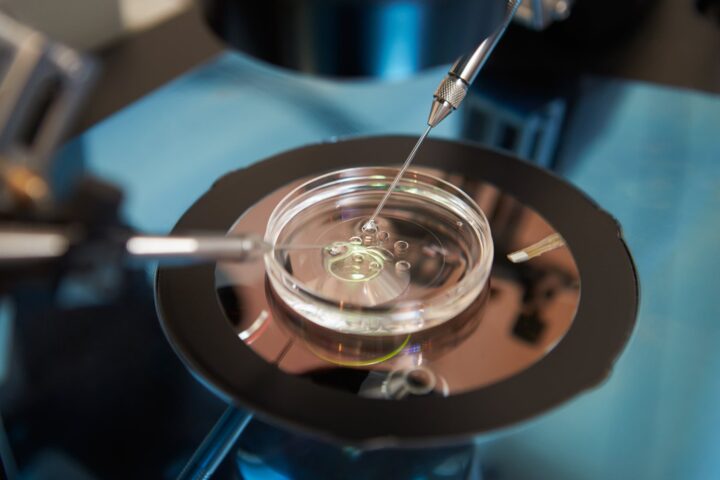
In simple terms, after three years of trying, we can expect less than 1 per cent per month (or cycle) conception rate. This background probability gives us a statistical expectation upon which we can compare the success, or otherwise, of all currently available treatments. Indeed, to consider an extreme example, we can increase a couple’s likelihood of conception by up to thirty-fold per cycle by doing IVF after three years of trying, providing they meet the other necessary criteria.
There are many other ways of expressing these statistics such as the ‘mean fecundity rate – MFR’ etc., but it has been shown repeatedly that of all the methods of predicting the ultimate likelihood of conception, independent of all other factors and causes, the time that a couple has been trying is the most useful single predictor of their likelihood of success if they are left untreated.
It is important however to view community ‘averages’ with caution, just as it is irrelevant to you reading this that the average age in the world today is 5.9 years. We must have a holistic approach and look at every couple’s situation carefully. Factors which are not ‘diseases’ per se are however vitally important and will now be reviewed. (The many ‘medical’ causes and available treatments are described in other AccessAustralia fact sheets.)
Age
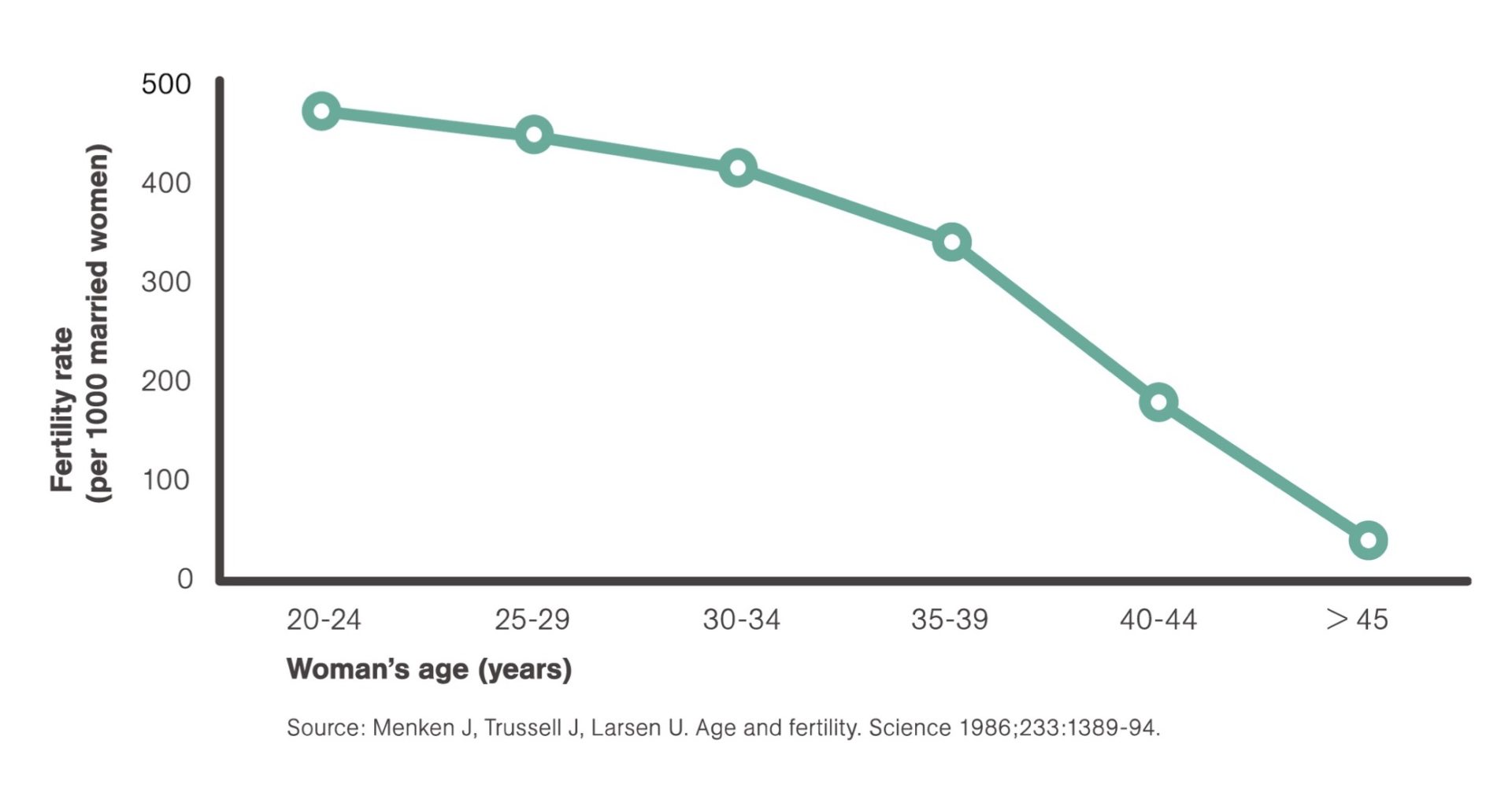
Most people are aware that fertility decreases with age. Factors that could contribute are the usual coincident increasing age of the partner (a factor mostly related to coital frequency) and the higher likelihood of having developed other conditions or disease(s) over time. However, a useful analysis of women receiving donor insemination, which can correct for these variables, confirms a most important age-specific decrease in fertility. Further, Menken et al. show very strong statistical support below in their classical and frequently cited article.
Women are born with a fixed (very large) number of oocytes (eggs) but the decline in fertility does not simply represent the dying off of these oocytes but, much more likely, their ageing and the continued environmental assault which makes them less ‘competent’. It is true to say that a woman’s 37th birthday marks a watershed in her reproductive potential. A societal trend in delaying child-bearing is therefore becoming significant in many western countries. There are sound reasons to encourage couples to start trying earlier and to treat the ‘older’ ladies more vigorously when they attend. With increasing age the miscarriage and fetal abnormality rate also increases adding further concerns.
Coital Frequency
The ‘window’ of conception is open from approximately two days before and until one day after oocyte release (ovulation). Intercourse at this time in women’s cycles yields the most pregnancies and, as an aside, the timing of intercourse before or after ovulation has no effect whatsoever on whether the infant will be male or female. The right time however is not always simple to determine without aids such as symptothermal charts (often called basal temperature charts) and/or simple hormonal monitoring but most pregnancies occur in those couples having intercourse three times per week around mid-cycle. Too much activity may result, for some men, in low sperm numbers being available and too little activity might miss the ‘window’. Other emotional issues of ‘making babies’ rather than ‘making love’ might also
be implicated and should be addressed sympathetically.
Smoking
The exact mechanism remains controversial but there is no doubt that smoking is associated with impaired fertility, increased miscarriages, ectopic (tubal) pregnancies, earlier onset of menopause, poorer pregnancy outcomes and, somewhat surprisingly, a decreased fertility in children born to mothers who smoke. It is disappointing to note that young women remain the only growing group of smokers. Recreational drugs such as marijuana render the user approximately half as likely to fall pregnant in a 12-month period as non-users. Stronger recreational drugs can have more major effects.
The message – don’t smoke – anything!
Exercise and diet
Extremes of faddism in foods and exercise are well recognised as a cause of menstrual irregularity and infertility but less extreme lifestyle changes also have an impact and this seems more related to neuroendocrine (brain hormone) changes rather than direct ovarian changes. Although there are different causes for ovulation disturbances from the overand under- weight, the end-result, i.e. impaired fertility, is similar. Fertility is maximal in those closest to ‘ideal’ body weight who exercise sensibly. Obesity in our community is a major factor in infertility. Another area often discussed is caffeine usage. Despite early, poorly controlled studies suggesting negative effects of caffeine, subsequent studies appear to suggest it is not a significant risk factor for infertility. Many therapeutic (prescription) drugs can contribute to infertility by a number of varying mechanisms and this should be discussed with the prescriber. Many herbal and ‘natural’ therapies also contain hormones, e.g. phytoestrogens that may interfere with fertility and should be taken with care when conception is desired. Most complementary medicine practitioners understand this but it is always prudent to ask.
Stress
Anecdotes abound regarding the success of ‘relaxing’, adopting a child and having holidays. Sadly, it is not that simple and there is very little statistical support for such claims. There is little doubt that a delay or inability to conceive causes itself a great deal of stress but well controlled psychometric observations have failed to define any causal relationship between emotion and infertility. This, however, is not to diminish the importance of empathetic, sensitive, professional assistance by health providers.
Summary
This fact sheet sets out to define some ‘normative’ data upon which realistic expectations of the likelihood of conception can be based. It is only by understanding such data that appraisals of available treatment options can be properly evaluated. Factors such as tubal disease, ovulatory disturbances and
sperm problems are discussed in other AccessAustralia fact sheets but we should never overlook fundamental factors such as age, coital frequency, smoking, exercise and diet.
Professor Geoffrey Driscoll
For more information visit access.org.au
Source: Australia’s National Infertility Network | Access Australia – ‘A rational definition of infertility’